ECG Training for Nurses: Building Confidence in Cardiac Monitoring from Acquisition to Interpretation
A comprehensive guide to building and maintaining ECG competency in nursing practice. Learn both acquisition technique and interpretation fundamentals.
The ECG Competency Gap in Nursing
ECG competency is one of the most critical—and most undertrained—skills in nursing. Surveys consistently show that nurses report low confidence in ECG interpretation, and even fewer have received formal training on ECG acquisition: the physical act of placing electrodes and obtaining a quality tracing.
Yet nurses are often the first clinicians to acquire an ECG when a patient presents with chest pain, shortness of breath, or altered mental status. In emergency departments, med-surg floors, and critical care units, the nurse's ability to quickly obtain an accurate 12-lead ECG can directly affect patient outcomes. Getting it right matters.
This isn't a failure of individual nurses—it's a systemic failure in how we train and support clinical staff. Most nursing programs dedicate only a few hours to ECG, with the overwhelming focus on rhythm interpretation rather than acquisition technique. Ongoing competency assessment is rare. Nurses are expected to be proficient, but they're rarely given the tools, training, or feedback to develop genuine expertise.
The good news: these gaps can be closed. With the right approach to training—and the right technology to support it—nurses can build confidence and competence in both ECG acquisition and interpretation.
ECG Acquisition: The Skill Nurses Aren't Taught
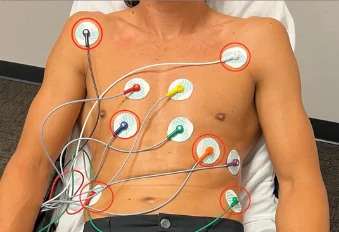
Why Electrode Placement Matters as Much as Interpretation
Here's a fundamental truth that many training programs overlook: you can't interpret what you can't acquire correctly.
An ECG with misplaced electrodes doesn't just look different—it can show pathology that doesn't exist or hide pathology that does. Research shows that 94.2% of ECG acquisitions have at least one misplaced electrode (Gregory et al., 2021). This rate includes nurses, paramedics, technicians, and physicians. The problem is universal.
The consequences are real:
- V1/V2 placed one intercostal space too high can create false ST elevation that mimics a STEMI
- Misplaced lateral leads can mask genuine ischemia
- Limb lead reversal can simulate dextrocardia or confuse rhythm interpretation
- Poor electrode contact creates artifact that may be mistaken for arrhythmia
When a nurse acquires an ECG, they're not just collecting data—they're creating the foundation on which all subsequent clinical decisions will be made. Placement accuracy directly determines diagnostic accuracy.
Practical Acquisition Tips for Nurses
Finding the fourth intercostal space: This is where most errors occur. Palpate the sternal angle (Angle of Louis)—the ridge where the manubrium meets the sternal body. The second rib articulates here. Move your fingers laterally to the second intercostal space, then count down two more spaces to reach the fourth intercostal space. V1 and V2 go here, flanking the sternum.
Adapting to body habitus:
- On obese patients, landmarks may be obscured. Take extra time, use multiple reference points, and don't be afraid to ask for help or a second opinion
- On female patients, V4-V6 should be placed under the breast, not over it. Placement over breast tissue attenuates the signal
- On very thin patients, be careful not to place electrodes directly over ribs—this reduces signal amplitude
Skin preparation: Proper prep dramatically improves tracing quality. For diaphoretic patients, wipe the skin dry. For patients with significant chest hair, clipping (not shaving, which can cause microabrasions) improves adhesion. A quick abrasion with a prep pad removes dead skin cells and improves electrode contact.
Troubleshooting artifact: When you see baseline wander or high-frequency noise, systematically check:
- Electrode adhesion—are they firmly stuck?
- Cable connections—are they secure?
- Patient position—is the patient moving or shivering?
- Electrode age—old or dried-out electrodes lose conductivity
For a complete guide to proper 12-lead ECG placement technique, see our detailed clinical guide.
ECG Interpretation Fundamentals Every Nurse Needs
A Systematic Approach to Reading an ECG
The key to ECG interpretation is having a systematic approach you apply every single time. This prevents you from fixating on obvious findings while missing subtle but important ones.
A simple framework:
- Rate: Is it normal (60-100), brady (<60), or tachy (>100)?
- Rhythm: Is it regular? Are there P waves? Is the P-QRS relationship consistent?
- Axis: Is the electrical axis normal, or is there left or right axis deviation?
- Intervals: Are PR, QRS, and QT intervals within normal limits?
- Segments: Is the ST segment at baseline, elevated, or depressed?
- Morphology: Are there Q waves, tall R waves, inverted T waves, or other waveform abnormalities?
Applying this framework consistently builds pattern recognition over time. You'll start seeing abnormalities intuitively, but the systematic approach ensures you don't miss anything.
Critical Rhythms and Red Flags
Rhythms every nurse must recognize immediately:
- Ventricular fibrillation: Chaotic, no organized QRS—requires immediate defibrillation
- Ventricular tachycardia: Wide complex tachycardia—potentially unstable, may require cardioversion
- Asystole: Flat line (after confirming it's not lead disconnect)
- Third-degree (complete) heart block: P waves and QRS complexes marching independently—may require pacing
- STEMI: ST elevation in contiguous leads—time-critical, every minute matters
When to notify the physician immediately:
- Any new arrhythmia with hemodynamic instability
- New ST elevation or depression
- New wide complex tachycardia
- Complete heart block or high-grade second-degree block
- Significant rate changes with symptoms
Artifacts vs. Pathology: Knowing the Difference
One of the most important skills is distinguishing artifact from real ECG changes. Common artifacts that can mimic pathology:
- Muscle tremor (Parkinsonian tremor, shivering): Can look like atrial fibrillation or flutter
- Loose electrode: Can create baseline wander or intermittent spikes that mimic ectopy
- 60 Hz interference: Creates a regular, fine oscillation throughout the tracing
- Patient movement: Can create large deflections that might be mistaken for PVCs or other ectopy
Key principle: Always correlate the ECG with the patient. If the tracing shows ventricular fibrillation but the patient is sitting up talking to you, check your leads before calling a code.
Building an Effective ECG Training Program
Core Components of Nurse ECG Education
Effective ECG training programs include both acquisition and interpretation, with hands-on practice and ongoing assessment:
1. Baseline assessment: Start by understanding what nurses already know (and don't know). A pre-training assessment identifies specific knowledge gaps to address.
2. Structured didactic education:
- Acquisition technique (often neglected—don't skip this)
- Basic rhythm interpretation
- Recognition of critical findings
- Artifact identification and troubleshooting
3. Hands-on practice with feedback: Simulation labs, supervised ECG acquisition on real patients with immediate feedback, practice strips with guided interpretation.
4. Regular competency reassessment: Not just once during orientation—ongoing assessment ensures skills are maintained and gaps are identified before they affect patient care.
Resources for ECG education:
- American Heart Association courses (ACLS, PALS include ECG components)
- Online ECG training platforms
- Simulation-based training programs
- CBI's training videos for device-specific acquisition technique
Ongoing Competency Assessment
Initial training fades without reinforcement. Best practices for ongoing competency include:
- Annual written assessments covering both acquisition and interpretation
- Periodic observed ECG acquisition with feedback from a qualified preceptor
- Quality metrics tracking repeat ECG rates, artifact rates, and acquisition-to-interpretation time
- Peer review and case discussions that include ECG review
- Access to reference materials and just-in-time learning resources at the point of care
How Technology Is Changing ECG Training and Accuracy
The traditional approach to ECG training assumes that nurses will eventually master anatomical landmark identification through repetition and experience. But with 94.2% of ECGs showing at least one misplaced electrode, this assumption doesn't hold.
Technology can support both training and ongoing accuracy:
Guided placement systems: The EXG platform incorporates anatomical markers that guide correct electrode positioning. This serves a dual purpose: it improves accuracy immediately while also teaching correct technique through consistent reinforcement. Nurses using the system learn where electrodes should go because the device shows them—every time.
Reduced cognitive load: In CBI's clinical studies, providers reported strong agreement on ease of use and reduced mental effort when using the EXG compared to traditional electrode placement. When the tool handles the complexity of electrode positioning, nurses can focus on the patient.
Standardization across providers: One of the biggest challenges in ECG training is ensuring that all nurses in a department achieve consistent results. When the technology guides placement, the variability between providers drops dramatically—from 60 misplaced electrodes with traditional setup to just 3 with the EXG in clinical studies.
For departments seeking to improve ECG competency while supporting their nursing staff, combining structured training with placement-guided technology offers a practical path forward.
Ready to explore how the EXG can support your training program? Contact us for a consultation, review our clinical evidence, or watch our training videos to see the system in action.
Common Placement Challenge Areas
Acquisition Knowledge Gaps
Common areas where nurses lack formal training
- Identifying correct intercostal spaces for precordial leads
- Adapting placement for different body types
- Proper skin preparation techniques
- Recognizing artifact vs. real ECG changes
- When and how to acquire right-sided or posterior leads
- Quality assessment of the completed tracing
Interpretation Confidence
Areas where nurses report low confidence
- Differentiating SVT from ventricular tachycardia
- Recognizing subtle ST changes
- Understanding axis deviation significance
- Identifying bundle branch blocks
- Distinguishing paced rhythms from intrinsic
- Correlating ECG findings with clinical presentation
System-Level Training Barriers
Organizational challenges to ECG education
- Nursing school provides limited ECG curriculum
- Hospital orientation ECG training is brief and surface-level
- No ongoing competency reassessment after orientation
- High nurse turnover creates constant training demand
- Lack of standardized placement protocols
- Training tools haven't kept up with clinical demands
ECG Competency Self-Assessment for Nurses
Honestly assess your current ECG knowledge and skills. Check any areas where you feel you could use more training or practice.
Acquisition Skills
Frequently Asked Questions
Combine structured education (courses, online learning) with hands-on practice and regular competency assessment. Focus on both acquisition technique and interpretation skills, and use technology that provides real-time guidance on electrode placement to reinforce correct technique.
Nurses need training in both ECG acquisition (electrode placement, skin preparation, quality assessment) and interpretation (systematic reading approach, rhythm recognition, identifying critical findings). Most programs underemphasize acquisition, which is the foundation of accurate interpretation.
Best practice is initial competency assessment during orientation, followed by annual reassessment. Departments with high acuity or high ECG volume should consider more frequent evaluation and ongoing education. Quality metrics tracking (repeat ECG rates, artifact rates) provide ongoing performance feedback.
At minimum, nurses should reliably identify normal sinus rhythm, atrial fibrillation, atrial flutter, SVT, ventricular tachycardia, ventricular fibrillation, asystole, heart blocks (first, second, and third degree), and STEMI patterns. Priority depends on clinical setting—ICU nurses need deeper arrhythmia knowledge than med-surg nurses.
Yes. Systems that use anatomical markers and guided placement (like the EXG) reduce reliance on manual landmark identification, which is the primary source of placement errors. These tools improve accuracy while simultaneously reinforcing correct technique—serving as both a training tool and a permanent solution.
Ready to Improve ECG Accuracy?
See how the EXG platform can standardize electrode placement across your organization.

