12-Lead ECG Placement: The Complete Guide for Clinicians & EMS Providers
Master the fundamentals of 12-lead ECG electrode placement with this comprehensive guide covering anatomical landmarks, common mistakes, and how to ensure diagnostic accuracy.
Why Accurate 12-Lead ECG Placement Matters More Than You Think
Every day, thousands of 12-lead ECGs are acquired in emergency departments, ambulances, and clinics worldwide. Yet studies consistently reveal a troubling reality: electrode misplacement occurs in up to 94.2% of ECG acquisitions according to Gregory et al. (2021). This isn't just a technical issue—it's a patient safety concern that can lead to missed heart attacks, false STEMI activations, and delayed treatment.
Research published in the Journal of Electrocardiology found that only 5.8% to 41.6% of paramedics demonstrated correct placement of all electrodes on manikins. Similar studies show that 64% of nurses and nearly 80% of cardiologists (specifically for V1 and V2 leads) struggle with proper precordial electrode positioning. When even cardiologists make these errors, it underscores how challenging accurate placement truly is—and why EMS providers and hospital staff need better tools.
The consequences extend far beyond documentation. Research shows that as little as 2 cm of electrode misplacement can mask the signs of a heart attack. A single misplaced electrode can also transform a normal ECG into one that mimics a STEMI—in fact, 72% of unnecessary cath lab activations are attributed to ECG-related factors including electrode misplacement. Each false activation costs healthcare systems tens of thousands of dollars, not to mention the risk and stress imposed on patients.
The Complete 12-Lead ECG Electrode Placement Guide
A standard 12-lead ECG uses 10 electrodes to generate 12 different views of the heart's electrical activity. Understanding the precise anatomical landmarks for each electrode is fundamental to obtaining diagnostically accurate tracings.
Limb Lead Placement (RA, LA, RL, LL)
The four limb electrodes measure electrical activity in the frontal plane and should be placed on the limbs—not on the torso. While some protocols allow torso placement for convenience, this can alter waveform morphology and should be documented.
- RA (Right Arm): Inner aspect of the right wrist, or right shoulder if using torso placement
- LA (Left Arm): Inner aspect of the left wrist, or left shoulder if using torso placement
- RL (Right Leg): Above the right ankle on the inner leg, or right lower abdomen if using torso placement (this is the ground electrode)
- LL (Left Leg): Above the left ankle on the inner leg, or left lower abdomen if using torso placement
Clinical tip: Ensure electrodes are placed on fleshy areas with good contact, avoiding bony prominences where the signal may be weak or artifact-prone.
Precordial Lead Placement (V1-V6)
The six precordial (chest) leads provide views of the heart in the horizontal plane. Accurate placement requires palpation of anatomical landmarks—a skill that takes practice to master.
- V1: Fourth intercostal space, right sternal border
- V2: Fourth intercostal space, left sternal border
- V3: Midway between V2 and V4 (requires placing V4 first)
- V4: Fifth intercostal space, midclavicular line
- V5: Same horizontal level as V4, anterior axillary line
- V6: Same horizontal level as V4 and V5, midaxillary line
Finding the fourth intercostal space: Palpate the sternal angle (Angle of Louis)—the ridge where the manubrium meets the sternal body. The second rib articulates here. Move your fingers laterally to the second intercostal space, then count down two more spaces to reach the fourth intercostal space.
The Most Common ECG Placement Mistakes (And How They Affect Your Reading)
Understanding what goes wrong—and why—is the first step toward improving placement accuracy.
Precordial Lead Errors
V1/V2 placed too high: This is the most common error, occurring when electrodes are placed in the second or third intercostal space instead of the fourth. This can create the appearance of right bundle branch block patterns, anterior ST elevation, or R-wave progression abnormalities that don't actually exist.
V4-V6 not following the correct anatomical line: V5 and V6 should remain on the same horizontal plane as V4. Placing them too high or low creates inconsistent waveform morphology that complicates serial comparison.
Placement over bone: Electrodes placed directly over the sternum or ribs (rather than intercostal spaces) result in reduced signal amplitude and increased artifact.
Limb Lead Reversal
Reversing the right and left arm leads is one of the most common errors and creates a characteristic pattern: inverted P waves and QRS complexes in Lead I, with a positive deflection in aVR. This pattern can mimic dextrocardia or lead to complete misinterpretation of the rhythm.
Other limb lead reversals can create equally confusing patterns, making systematic lead application and verification essential.
Clinical Challenges That Make Accurate Placement Difficult
Body Habitus Variations
Obese patients: Chest wall adiposity makes palpating the sternal angle and intercostal spaces extremely difficult. The landmarks may be displaced, and chest wall thickness can attenuate signal amplitude. Consider using multiple reference points and taking extra time to verify landmarks.
Female patients: Breast tissue presents unique challenges. Current guidelines recommend placing V4-V6 under the breast rather than on top of it, as placement over breast tissue can attenuate the signal and alter waveform morphology. This requires clear communication and patient consent.
Patients with chest deformities: Pectus excavatum, pectus carinatum, and kyphoscoliosis can significantly alter the relationship between surface landmarks and cardiac position, requiring adaptive placement strategies.
Prehospital and Emergency Settings
EMS providers face additional challenges that hospital staff often don't encounter:
- Limited space in ambulances and helicopters
- Poor lighting conditions
- Patient movement during transport
- Time pressure during STEMI alerts or cardiac arrest
- Diaphoretic patients with poor electrode adhesion
- Hypothermic patients requiring layers to be removed
These factors contribute to the higher misplacement rates observed in prehospital settings compared to controlled hospital environments.
Inter-Rater Variability
Perhaps the most overlooked challenge is inconsistency between providers. When a patient receives an ECG in the field, another in the ED, and a third in the cath lab, three different providers may place electrodes in three different positions. This makes serial comparison—critical for detecting evolving ischemia—unreliable.
Studies have shown significant variation in where providers identify the same anatomical landmarks, even among experienced clinicians. This inter-rater variability undermines one of the ECG's most valuable capabilities: tracking changes over time.
The Real Consequences of ECG Misplacement
The clinical and operational impacts of electrode misplacement are substantial:
- False-positive STEMI activations: Precordial lead misplacement can create ST elevation that triggers cath lab activation for a patient without actual coronary occlusion. False activation rates at some centers exceed 25%, with each incident costing $10,000-$20,000 in resources.
- Missed acute MI: Conversely, improper placement can normalize pathological changes, causing providers to miss genuine cardiac events that require emergent intervention.
- Incorrect rhythm interpretation: Limb lead reversal and artifact from poor electrode contact can make accurate rhythm analysis impossible.
- Delayed treatment: When ECG quality is poor, repeat acquisitions are needed, delaying time-sensitive treatments in STEMI and cardiac arrest.
- Legal liability: Documentation of electrode placement is increasingly scrutinized in malpractice cases involving missed cardiac diagnoses.
How Technology Is Solving the Placement Problem
Recognizing that human factors contribute significantly to placement errors, innovators have developed technological solutions to standardize electrode positioning.
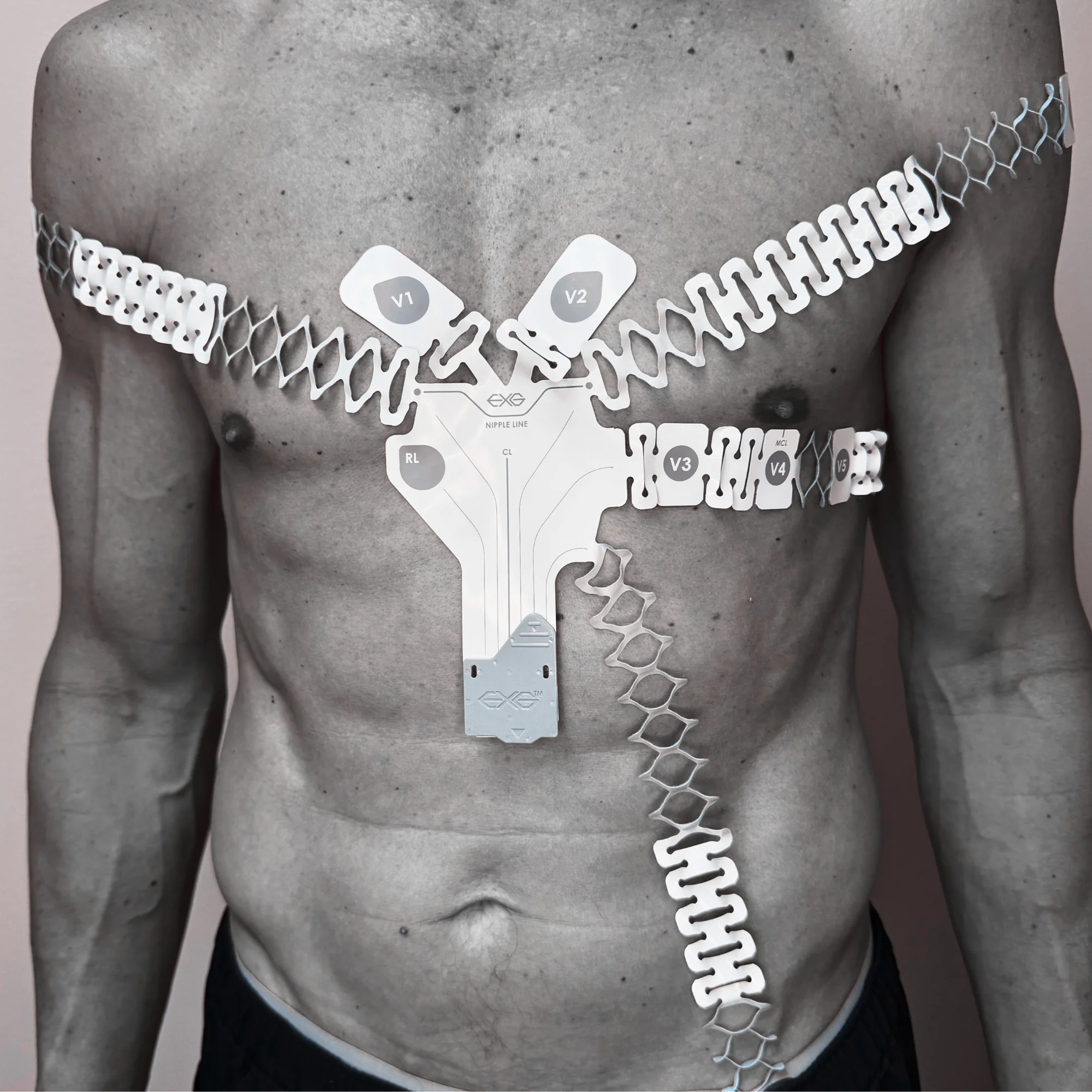
The EXG Wearable ECG Platform from C-Booth Innovations represents a paradigm shift in ECG acquisition. Rather than relying on providers to independently identify and mark 10 separate electrode positions, the EXG integrates all precordial electrode sites into a single anatomically-guided adhesive device.
Key features that address placement challenges:
- Anatomical markers: Screen-printed guidelines eliminate guesswork in electrode positioning
- Single reference point: Central placement over the sternum with alignment to the nipple line simplifies landmark identification
- Consistent inter-electrode spacing: Fixed geometry ensures V1-V6 maintain proper relationships regardless of provider
- Reduced setup complexity: Single connection terminal decreases cable confusion and lead reversal errors
- Radiolucent design: Allows continuous monitoring through X-rays, CT scans, and cath procedures without removal
Clinical studies have demonstrated dramatically improved inter-rater agreement with the EXG system. In one study comparing traditional electrode placement to the EXG platform, researchers found 60 misplaced electrodes with conventional leads versus only 3 with the EXG system—a 95% reduction in placement errors. For healthcare systems seeking to reduce false STEMI activations and improve diagnostic consistency, these innovations offer a practical path forward.
To learn more about how the EXG platform can support your cardiac monitoring protocols, request a demonstration, explore our clinical evidence, or watch our training videos to see proper application technique.
Common Placement Challenge Areas
Precordial Placement Errors
The most common and impactful electrode misplacements
- V1/V2 placed in wrong intercostal space (most common error)
- V4-V6 not following the anatomical line
- Inconsistent spacing between V1-V6
- Placement over bone instead of intercostal space
- Poor contact due to chest hair or diaphoresis
- Misidentification of anatomical landmarks
Limb Lead Challenges
Errors that fundamentally alter the ECG tracing
- Left arm / right arm lead reversal
- Leads placed on trunk instead of limbs
- Inconsistent placement location between acquisitions
- Cable tangling causing incorrect lead assignment
- Poor skin contact on extremities
- Movement artifact from loose electrodes
Environmental & Patient Factors
Real-world challenges that compound placement difficulty
- Obese patients — difficulty palpating landmarks
- Female patients — breast tissue displacement
- Diaphoretic patients — electrode adhesion failure
- Prehospital settings — confined space, poor lighting
- Time pressure during STEMI alerts
- Provider fatigue during long shifts
ECG Placement Quality Self-Assessment
How confident are you in your 12-lead placement technique? Check any challenges you've experienced or areas where you feel less confident.
Precordial Placement
Frequently Asked Questions
A 12-lead ECG requires 10 electrodes: four limb leads (RA on right arm, LA on left arm, RL on right leg, LL on left leg) and six precordial leads (V1-V6). V1 goes in the fourth intercostal space at the right sternal border, V2 in the fourth intercostal space at the left sternal border, V4 in the fifth intercostal space at the midclavicular line, V3 between V2 and V4, V5 at the anterior axillary line level with V4, and V6 at the midaxillary line level with V4 and V5.
Incorrect ECG lead placement can cause significant diagnostic errors. Misplaced precordial leads (especially V1/V2 placed too high) can create false ST elevation mimicking a STEMI, leading to unnecessary cath lab activations. Limb lead reversal can produce patterns that mimic dextrocardia or rhythm abnormalities. Misplacement can also mask real cardiac events, potentially delaying critical treatment for actual heart attacks.
V1 and V2 are both placed in the fourth intercostal space—V1 at the right sternal border and V2 at the left sternal border. To find the fourth intercostal space, locate the sternal angle (Angle of Louis), which is where the second rib articulates. From there, count down two intercostal spaces. This is the most commonly misplaced electrode position, with many providers incorrectly placing these leads in the second or third intercostal space.
For female patients, the American Heart Association recommends placing electrodes V4, V5, and V6 under the breast rather than on top of breast tissue. Breast tissue can attenuate the ECG signal and alter waveform morphology. Clear communication with the patient about lead placement is important for comfort and consent. The V1-V3 leads are typically not affected as they are placed medially on the chest.
Consistent electrode placement is critical for serial ECG comparison—one of the most valuable diagnostic capabilities of the 12-lead ECG. When electrodes are placed differently between acquisitions (by different providers or at different facilities), changes in waveform morphology may reflect placement variation rather than actual cardiac changes. This makes it difficult to track evolving ischemia or treatment response. Standardized placement systems help ensure reproducibility across providers and settings.
Ready to Improve ECG Accuracy?
See how the EXG platform can standardize electrode placement across your organization.

