ECG Electrode Placement: How Small Errors Create Big Diagnostic Problems
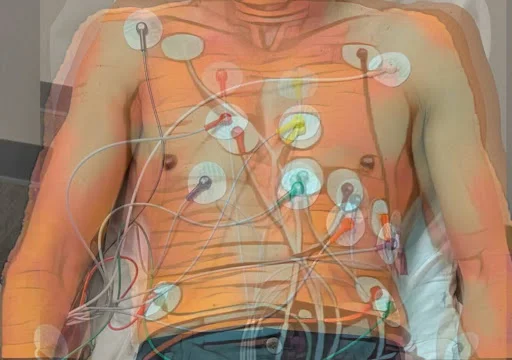
Understanding how electrode misplacement affects ECG interpretation and patient outcomes. Learn about the diagnostic cascade from a single misplaced electrode to unnecessary interventions.
When a Misplaced Electrode Activates the Cath Lab
A 58-year-old man arrives at the emergency department with chest pain. The nurse acquires a 12-lead ECG, and the physician sees what appears to be ST elevation in leads V1 and V2—the hallmark of an anterior STEMI. The cath lab is activated. The interventional cardiologist arrives within minutes, the patient is prepped, and the catheter is advanced into the coronary arteries.
The arteries are clean. No occlusion. No culprit lesion. The patient never had a heart attack.
What happened? The precordial electrodes were placed one intercostal space too high—a common error that created the appearance of ST elevation where none existed. The patient underwent an invasive procedure with real risks, the healthcare system absorbed $15,000-$25,000 in costs, and the cath lab was occupied for a non-emergent case while another patient with a real STEMI might have been waiting.
This scenario plays out in hospitals every day. It's not a rare occurrence—it's a systemic problem that stems from fundamental issues with how we acquire ECGs.
The Scope of ECG Electrode Placement Errors
The extent of electrode misplacement in clinical practice is staggering. Research by Gregory et al. (2021) found that 94.2% of ECG acquisitions had at least one misplaced electrode. This isn't a problem limited to inexperienced providers—studies show that nurses, paramedics, technicians, and even cardiologists struggle with consistent electrode placement.
Perhaps more concerning is the gap between provider confidence and actual performance. In CBI's own research, providers reported high confidence in their placement technique, yet objective measurement revealed significantly more misplacements than they realized. This disconnect means the problem persists undetected—providers don't know what they don't know.
The downstream effects are substantial. 72% of unnecessary cath lab activations are attributed to ECG-related factors, with electrode misplacement being a primary contributor. Each false activation costs healthcare systems $10,000-$25,000 or more, but the true cost extends beyond dollars to patient risk, system capacity, and provider burnout.
How Specific Electrode Errors Change Your ECG Tracing
Precordial Lead Misplacement Effects
V1/V2 placed too high (most common error): When V1 and V2 are placed in the second or third intercostal space instead of the fourth, the electrodes are positioned closer to the right ventricular outflow tract. This can create:
- False ST elevation mimicking an anterior STEMI
- rSr' pattern that mimics Brugada syndrome (a potentially lethal arrhythmia condition)
- Apparent right bundle branch block pattern that doesn't exist
- Abnormal R-wave progression that suggests anterior wall damage
The clinical implications are severe. A false Brugada pattern can lead to unnecessary implantable defibrillator placement. A false STEMI can lead to emergent catheterization. Both expose patients to real procedural risks for conditions they don't have.
V4-V6 displaced laterally or vertically: These leads are meant to capture the lateral wall of the left ventricle. When mispositioned:
- R-wave progression becomes unreliable
- Lateral wall ischemia may be masked or mimicked
- Serial ECG comparison becomes meaningless
Limb Lead Reversal Patterns
Right arm / left arm reversal: This creates a characteristic pattern with Lead I appearing inverted—negative P wave, negative QRS, and the ECG axis appearing markedly abnormal. This pattern can mimic dextrocardia (a rare condition where the heart is on the right side of the chest) or lead to complete misinterpretation of the cardiac rhythm.
Right leg / left leg reversal: Creates a more subtle abnormality that may not be immediately recognized, potentially causing rhythm misinterpretation or axis miscalculation.
Contact Quality and Signal Degradation
Electrodes placed over bone: When electrodes sit directly on the sternum or ribs rather than in the intercostal spaces, signal amplitude drops and artifact increases. The resulting tracing may show:
- Low voltage that mimics pericardial effusion or obesity
- Baseline wander that obscures ST segment analysis
- Muscle artifact that can mimic atrial fibrillation or ventricular tachycardia
The Diagnostic Cascade: From Misplacement to Patient Impact
Understanding how a single placement error propagates through the diagnostic chain reveals why this problem matters so much.
The cascade unfolds:
- Misplaced electrode → V1/V2 one intercostal space too high
- Abnormal tracing → ST elevation appears in anterior leads
- Clinical decision → Physician interprets as anterior STEMI
- System activation → Cath lab team called in, patient consent obtained
- Invasive procedure → Catheterization performed with contrast and radiation exposure
- Discovery → Clean coronaries found, no intervention needed
- Consequences → Patient risk, system cost ($15,000-$25,000+), occupied resources
But the cascade can flow the other direction with equally devastating consequences:
- Misplaced electrode → V3-V6 positioned too high or laterally
- Masked pathology → Real ST elevation is normalized by the misplacement
- Clinical decision → Physician sees "normal" ECG, rules out STEMI
- Delayed treatment → Patient doesn't receive emergent reperfusion
- Outcome → Larger infarct, worse prognosis, potential death
Research has established that as little as 2 cm of electrode misplacement can mask the signs of a heart attack (Bond et al., 2012). In STEMI, every minute of delay increases mortality by approximately 2%. A placement error that delays recognition by even 30 minutes can measurably affect patient survival.
Why ECG Electrode Placement Errors Persist
Outdated Technology
The fundamental design of ECG electrode systems hasn't meaningfully changed since the 1950s. Providers are still expected to identify multiple anatomical landmarks, apply discrete electrodes in precise positions, manage multiple cables, and do this consistently across thousands of patients with varying body habitus—all while under time pressure. The technology has simply not evolved to support reliable human performance.
Training Gaps
Medical and nursing education overwhelmingly emphasizes ECG interpretation over ECG acquisition. Clinicians spend hours learning to read rhythms and ST changes, but may receive only cursory instruction on proper electrode placement technique. The assumption is that acquisition is simple—but the data clearly shows it is not.
Ongoing competency assessment for ECG acquisition is rare. Most providers receive placement training during initial orientation and never again. There's no systematic feedback loop to identify and correct placement errors before they affect patient care.
Unrecognized Inter-Rater Variability
Perhaps the most insidious factor is that providers don't realize how much their placement varies from their colleagues. When a patient receives an ECG from three different providers across the care continuum—field, ED, cath lab—they may effectively receive three different ECGs. This destroys the ability to track changes over time, which is one of the ECG's most valuable diagnostic capabilities.
Studies have shown that even experienced clinicians identify the same anatomical landmarks in significantly different locations. Without a standardization mechanism, this variability is inevitable.
Standardizing ECG Electrode Placement to Eliminate Errors
Recognizing that human factors are the core driver of placement errors, C-Booth Innovations developed the EXG platform to fundamentally redesign how ECGs are acquired.
Rather than relying on providers to independently identify and mark 10 separate electrode positions, the EXG integrates all precordial electrode sites into a single anatomically-guided adhesive device. Screen-printed markers guide placement to a single reference point, eliminating the guesswork and inter-rater variability inherent in traditional approaches.
The results speak for themselves: In clinical studies comparing traditional electrode placement to the EXG system, researchers documented 60 misplaced electrodes with conventional leads versus only 3 with the EXG system—a 95% reduction in placement errors (p<0.001).
Beyond accuracy, providers reported:
- Strong agreement on ease of use
- Reduced mental effort during acquisition
- Faster setup time in time-critical situations
- Greater confidence in ECG quality
For EMS systems, hospital EDs, and cath labs seeking to reduce false STEMI activations, improve diagnostic accuracy, and standardize care across providers, the EXG offers a practical path forward.
Ready to see how the EXG can transform your ECG acquisition workflow? Request a demonstration or explore our clinical evidence. For training resources on optimal ECG acquisition technique, visit our training videos.
Common Placement Challenge Areas
Tracing Artifacts from Misplacement
How electrode errors manifest on the ECG
- False ST elevation mimicking STEMI
- Pseudo-Brugada pattern from high V1/V2
- Altered R-wave progression
- Artificial axis deviation from limb reversal
- Reduced signal amplitude from bone contact
- Movement artifact from poor adhesion
Clinical Consequences
Real patient impacts of electrode errors
- Unnecessary cath lab activations ($10K-$25K+ each)
- Missed acute myocardial infarctions
- Delayed reperfusion therapy
- Incorrect rhythm interpretation
- Serial ECG comparison invalidated
- Increased medical-legal exposure
Systemic Contributing Factors
Why these errors continue to occur
- ECG technology unchanged since the 1950s
- Training focuses on interpretation over acquisition
- No built-in placement verification
- High inter-rater variability
- Time pressure in acute settings
- Provider overconfidence in technique
ECG Acquisition Error Risk Assessment
How exposed is your department to ECG placement errors? Check any that apply to your clinical setting.
Protocols & Standards
Frequently Asked Questions
Studies show electrode misapplication rates as high as 94.2%. Most providers are unaware of their own placement variability, and research demonstrates a significant gap between provider confidence and actual placement accuracy.
Yes. V1/V2 placed one intercostal space too high can produce ST elevation mimicking an anterior STEMI, potentially triggering unnecessary cath lab activation. This is one of the most clinically significant consequences of electrode misplacement.
Placing V1 and V2 too high (in the 2nd or 3rd intercostal space instead of the 4th) is the most frequently documented error. This mistake is so common because the anatomical landmarks can be difficult to identify, especially in patients with obesity or unusual chest wall anatomy.
Even a 2cm displacement can mask or mimic pathology. Research shows that misplacement can hide heart attacks or create false positive findings that lead to invasive procedures. The effect depends on which electrode is misplaced and in what direction.
Implementing standardized placement systems, regular training, and technology solutions that guide electrode positioning (like anatomical marker-based systems) have shown significant reduction in error rates. The EXG platform demonstrated a 95% reduction in placement errors compared to traditional electrodes.
Ready to Improve ECG Accuracy?
See how the EXG platform can standardize electrode placement across your organization.

